Call us toll-free: 800-878-7828 — Monday - Friday — 8AM - 5PM EST

Jayme Fraser and Matt Wynn for USA TODAY
No state in the U.S. will have enough room to treat novel coronavirus patients if the surge in severe cases here mirrors that in other countries.
A USA TODAY analysis shows that if the nation sees a major spike, there could be almost six seriously ill patients for every existing hospital bed.
That analysis, based on data from the American Hospital Association, U.S. Census, CDC and World Health Organization, is conservative. For example, it assumes all 790,000 beds will be empty.
Since two thirds are not, the reality could be far worse: about 17 people competing for each open bed.
“Unless we are able to implement dramatic isolation measures like some places in China, we’ll be presented with overwhelming numbers of coronavirus patients – two to 10 times as we see at peak influenza times,” said Dr. James Lawler, who researches emerging diseases at the University of Nebraska Medical Center and the Global Center for Health Security.
Lawler added that “no hospital has current capacity to absorb that” without taking crisis care measures, such as postponing elective procedures and reserving finite resources for those coronavirus patients most likely to recover.
USA TODAY’s analysis estimates 23.8 million Americans could contract COVID-19, the illness caused by the novel coronavirus that first appeared in Wuhan, China. That number is based on an infection rate of 7.4% – similar to a mild flu year.
Experts say this infection rate is likely to be far higher.
The Johns Hopkins Center for Health Security estimates that 38 million Americans will need medical care for COVID-19, including as many as 9.6 million who will need to be hospitalized – about a third of whom might need ICU-level care. In a February presentation to the American Hospital Association, Lawler estimated that as many as 96 million Americans could be infected.
The American Hospital Association wrote to congressional leaders in February to ask for money to build hospitals and housing to isolate patients.
Most people with COVID-19 will have only mild symptoms. Studies of cases in other countries suggest that some of those responsible for community spread were never identified as infected because they didn’t develop any symptoms.
But some still will need medical care – or at least medical isolation – at some point during the illness.
“In my case, it was like a very mild common cold,” said Carl Goodman, one of the passengers who picked up the virus while on the Diamond Princess cruise ship.
Goodman recently moved out of the biocontainment unit at the University of Nebraska Medical Center into a dorm-like monitoring room until he no longer tests positive for the virus.
The worst he felt was during the flight there from Travis Air Force Base in California.
“Suddenly, I had a 103-degree fever with no symptoms other than that,” he said. “No sore throat, no runny nose, no body aches or chills, no coughing. The coughing came later.”
For its analysis, USA TODAY used population figures from the Census and the number of hospital beds from the American Hospital Association. The AHA counts reflect figures from community hospitals – all nonfederal, short-term general facilities. It also includes academic medical centers and other teaching hospitals if they are nonfederal. It doesn’t include prison hospitals or college infirmaries.
The infection rate of novel coronavirus is still unclear. The analysis used that of a mild flu season. It also assumes that the 13.8% of patients with severe symptoms and 6.1% with critical symptoms would need hospitalization.
The World Health Organization defines a case of COVID-19 as severe if patients have shortness of breath, low blood oxygen, acute respiratory distress, and fluid buildup in their lungs. People in critical condition also experience respiratory failure, septic shock or multiple organ failure.
If everyone in the U.S. who gets that ill requires hospitalization, that would be 4.7 million patients – 5.7 for every domestic hospital bed.
That influx could be accommodated if it’s spread out over a long enough period of time but not if it comes as a rapid surge, as it did in the early stages of outbreak in China and Italy. In Italy, the virus overwhelmed the health care system in just three weeks.
“When hospitals become much more crowded, literally stretched beyond capacity, if I have a heart attack, will I be able to get care? If I have an auto accident, will I get care? How do we triage that?” said Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota.
“We can’t approach this like I approach a game of checkers with my 10-year-old grandson,” he added. “We have to approach this like a chess master thinking 10 to 15 moves down the board.”
Surge of new patients would overwhelm US hospitals quickly
A surge of new patients would be difficult any place in America. Many hospitals are designed to handle peak capacity during winter flu season, not an outbreak on top of that.
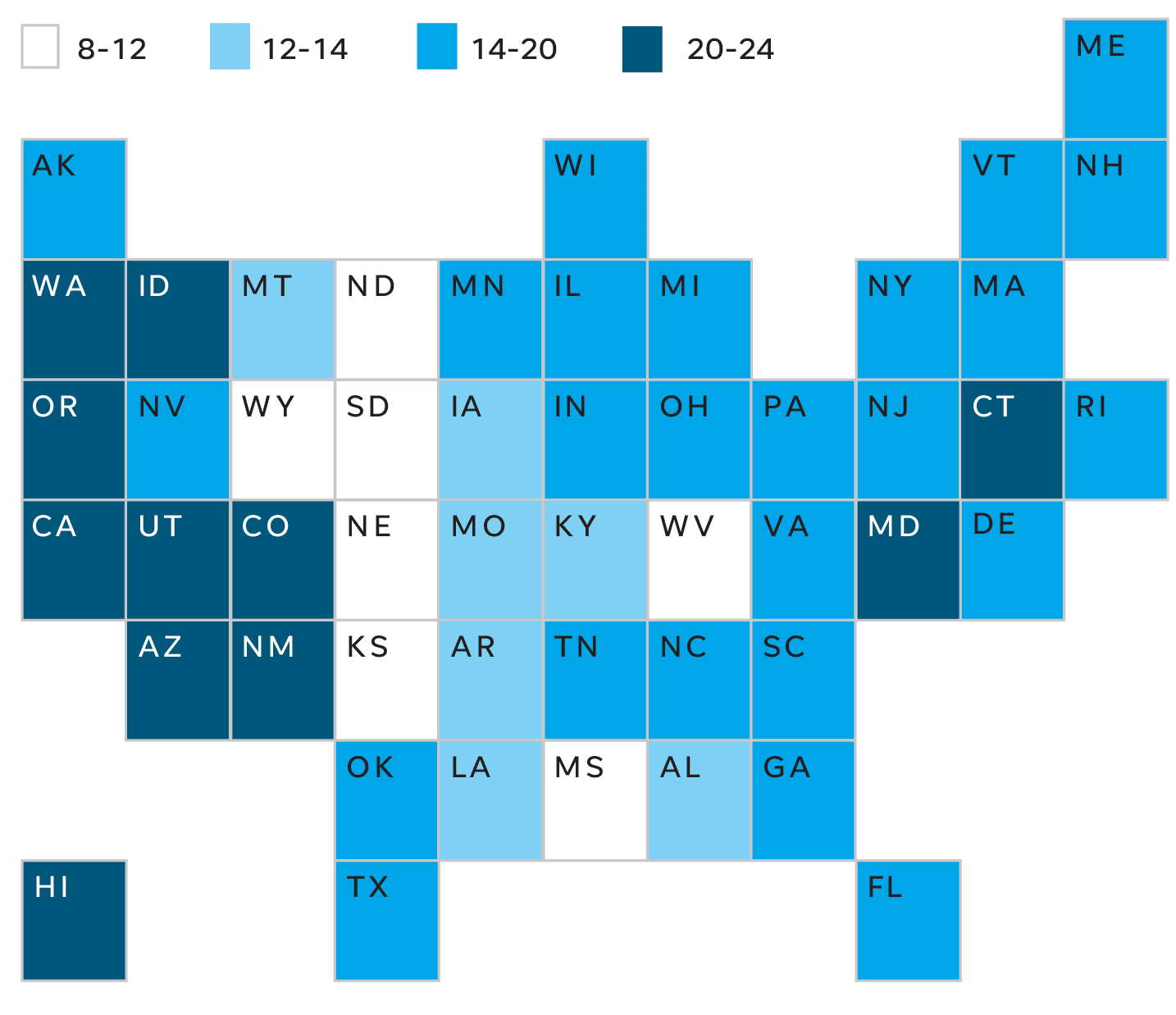
At the state level, the gaps between capacity and potential demand vary significantly.
Places like Oregon, Washington, New Mexico and California might need eight times as many beds, according to the USA Today analysis. South Dakota and North Dakota have the smallest gap between beds and potential need, but still could draw three patients for every bed.
But, given the beds already estimated to be in use, Oregon, Washington, New Mexico and California would need more than 20 times as many open beds. Even the states in the best shape – North and South Dakota, as well as Mississippi – could need 10 times more capacity.
Those figures assume the infections would happen all at once, which is unlikely, and that all beds are empty, when they are not. Nonetheless, experts say such estimates help pinpoint where it will be most critical to slow spread of the disease and develop robust emergency plans.
Dr. Gary Wheeler, medical director of infectious disease at the Arkansas Department of Health, said his state is aware that in an outbreak it would likely face shortages of not just beds, but staff and supplies.
Arkansas’ gap is among the smallest in the nation, according to the USA TODAY analysis. But a surge there still could dramatically overwhelm resources. About 44,000 people might need hospitalization in a state with about 9,500 beds, of which only about 3,400 are likely to be available on any given day.
If each person only needs to be hospitalized for 10 days – slightly less than the average in China – the state could manage if the cases were spread out over five months or more, the USA TODAY analysis shows. But if the surge compresses into four months or less, Arkansas would quickly run out of beds.
“We know that,” Wheeler said. “And our strategy is to delay the onset as much as possible so we will have relatively close to enough beds to meet the need as it comes in.”
States with large elderly populations will fall farther short
Focusing on the elderly, who are particularly vulnerable to complications from the virus, does not improve the outlook in most places.
Oregon – wedged between two states with hundreds of confirmed cases – appears to be at greatest risk for a shortage. The state would need more than twice as many beds as it has – 14,100 instead of 6,900 – to handle a surge of hospitalizations among its older population.
USA TODAY found that in a surge, only eight states would have enough hospital beds to treat the 1 million Americans 60 and older who could become seriously ill with COVID-19. Most were in the Midwest, in both North and South Dakota as well as Kansas, Kentucky, Louisiana, Nebraska, Mississippi and Wyoming.
All eight have significant rural populations served primarily by small hospitals, however, which typically are not equipped to handle multiple patients who need intensive care.
At the local level, about two-thirds of American cities would not have enough beds to serve residents 60 and older who became seriously ill. Based on an evaluation of about 400 metropolitan areas in the United States, some would need to increase their capacity fourfold or more.
For instance, New Mexico has four metropolitan areas: Santa Fe, Farmington, Las Cruces and Albuquerque. In those cities, the need to increase hospital capacity would range from 50% to 200% to accommodate people 60 or older.
Savannah, Georgia might be able handle an estimated surge of 1,060 serious COVID-19 cases among people 60 or older because the metro area reports nearly 1,300 hospital beds. But an hour southwest, Hinesville could see 150 cases for just 25 beds. A half hour northeast of Savannah is Bluffton, South Carolina, where there could be 961 serious cases for just 331 beds.
But, in a domino effect, Savannah could quickly be overwhelmed if either Hinesville or Bluffton transferred patients to their larger urban neighbor.
Already in Georgia, Gov. Brian Kemp said this week that “out of an abundance of caution” the state had started to isolate and monitor some people in emergency trailers set up at Hard Labor Creek State Park, which sits between Athens and Atlanta. Georgia reported its first death from the virus on Thursday.
The I-25 corridor of Colorado has potential for a similar overload, according to the analysis. Seven metropolitan areas from Fort Collins to Pueblo could be home to 13,000 older patients who need hospitalization. Yet, those cities together have just over 9,000 beds.
Preparing, and expanding hospital capacity, is key
Health officials cited many creative options for expanding capacity in an outbreak.
Hospital cafeterias can be filled with beds to become a makeshift isolation ward. So can other large buildings, such as school gyms.
Nurses can wheel a second bed into a private hospital room. Some hospitals’ emergency plans include setting up tents and cots in a parking lot, where they could triage incoming patients.
Dr. Susan Kline, infection prevention medical director for Minnesota Health Fairview, said public health officials there are developing guidelines for how to care for recovering COVID-19 patients at home.
“If a patient is symptomatically recuperated enough to go home they could be discharged even though they might not be 100%,” she said.
Dr. Colleen Kraft agreed that hospitals should think creatively about how to free up beds for those most in need.
“If people have to be quarantined or have to be isolated, we’re finding that healthcare’s being used as sort of safety net for that,” said Kraft, who leads the Clinical Virology Research Laboratory at Emory University School of Medicine. “And that’s not going to work if we have really sick people that need help.”
Hospitals also might choose to prioritize coronavirus care to gain beds typically reserved for other services. For instance, officials could cancel elective surgeries and convert the recovery unit into an isolation ward.
Before hospitals run out of beds, they could face problems finding enough qualified nurses, radiology and CT technicians, and intensive care doctors.
David Savitsky continues to run his medical staffing company from home, where he is self-isolating after being exposed to the virus. ATC Healthcare helps hospitals in 20 states find temporary workers and has seen an uptick in calls related to the new coronavirus amid an already busy flu season.
“Just yesterday I was on the phone with someone from a hospital where they need 75 nurses,” Savitsky said. “We’re going to be able to help them out to some extent; we’re not going to be able to get them 75 nurses.”
Emergency declarations could give governors the power to loosen certain professional standards or laws related to patient care. For instance, an intensive care unit that typically limits each nurse to caring for one or two patients might instead allow one nurse to monitor three patients.
States also also could provide temporary relief from laws that only recognize nursing licenses from a limited number of states, allowing hospitals to hire from a wider pool of professionals.
Dr. Lee Norman, secretary of the Kansas Department of Health and Environment, said a worst-case scenario would involve extremes never invoked, like rationing care among the coronavirus patients.
“It could lead to examining the probability of salvaging this patient and that patient,” he said. “It’s a little like in a battlefield. If somebody’s not going to make it, you make them comfortable as best you can.”
Mandatory community separation and isolation measures initiated quickly take pressure off of the hospitals by slowing the spread of coronavirus.
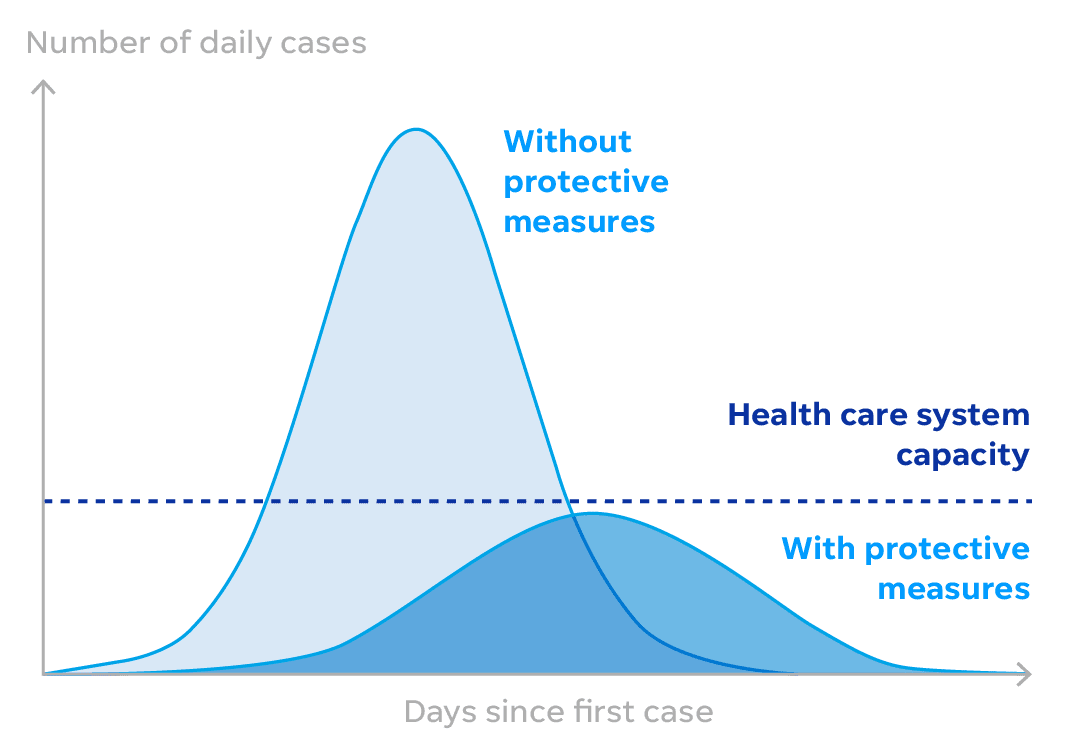
Lawler called that “the most powerful tool we have.” He pointed to the 1918 Spanish Flu pandemic as an example of how even a few days can make a difference.
In Philadelphia, “bodies were stacked on the sidewalk because they could not pick them up in time,” he said, while in St. Louis, residents had “a relatively benign experience and hospitals were not overwhelmed.”
“That difference between early and too late, between St. Louis and Philadelphia,” Lawler said, “appeared to be about two weeks.”
How we did this analysis
USA TODAY used population figures from the U.S. Census and the number of hospital beds from the American Hospital Association. The AHA counts reflect figures provided by community hospitals – all nonfederal, short-term general facilities. It also includes academic medical centers and other teaching hospitals if they are nonfederal but it doesn’t include places like prison hospitals or college infirmaries. Because the infection rate of novel coronavirus in this country remains unclear, the analysis used rates in a mild flu season. It also assumed that the 13.8% of patients with severe symptoms and 6.1% with critical symptoms all would need hospitalization. Since the World Health Organization reports that people 60 and over are most at risk, the analysis also focused on that population as reported by the Census.