Call us toll-free: 800-878-7828 — Monday - Friday — 8AM - 5PM EST
By Shelby Livingston for Modern Healthcare
Surprise out-of-network billing and related patients’ costs are increasing among inpatient admissions and emergency department visits to in-network hospitals, according to a study published Monday in JAMA Internal Medicine.
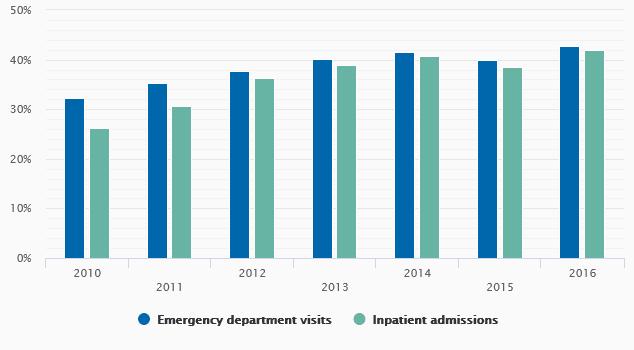
Stanford University researchers found that from 2010 through 2016, 39% of 13.6 million trips to the ED at an in-network hospital by privately insured patients resulted in an out-of-network bill. That figure increased during the study period from about a third of ED visits nationwide in 2010 to 42.8% in 2016.
Out-of-network billing among admissions to in-network hospitals occurred only slightly less often. Out of 5.5 million admissions, 37% of admissions resulted in at least one out-of-network bill during the entire seven-year period. The frequency increased from 26.3% in 2010 to 42% in 2016, according to the study.
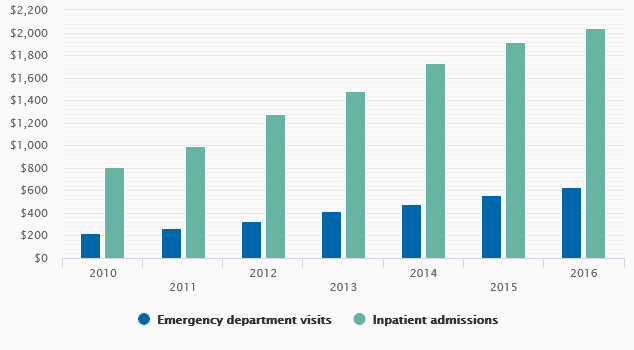
The average potential cost to patients associated with out-of-network bills more than doubled in both settings over the seven-year period.
Surprise billing is becoming more common
Out-of-network billing and associated patient costs for inpatient admissions and emergency department visits at in-network facilities increased over a six-year period.
Percentage of visits/admissions with out-of-network bill
The study adds to a growing body of evidence illustrating the frequency of and cost associated with surprise bills, which may occur when patients visit an in-network hospital and unknowingly receive care from an out-of-network physician. In recent months, surprise billing has received increased attention from lawmakers looking to shield patients from the big out-of-network bills.
Hospital and physician groups have lobbied thwart legislation that would cap out-of-network pay. Congress hopes to pass legislation addressing surprise billing in September.
“Our findings appear to support current efforts to strengthen legislative protections against out-of-network billing in circumstances that are likely to involve surprise bills,” the study authors concluded.
Researchers analyzed data from a single private health insurer. They found the cost to the patient associated with the surprise bills increased significantly during the study period. The patient’s potential financial responsibility from out-of-network ED bills grew from an average $220 in 2010 to $628 in 2016, though many patients’ bills far exceeded those averages. Those figures represent the difference between the amount charged by out-of-network physicians or ambulances, and the amount the insurer would pay in-network for the same service.
The potential cost to patients associated with out-of-network bills from inpatient admissions grew from an average $804 in 2010 to $2,040 in 2016. In 2016, however, the 90th percentile of patients with out-of-network bills faced potential costs of $4,112 or more.
Ambulances accounted for the most out-of-network bills among both ED visits and inpatient admissions. Researchers wrote that for patients who visited the ED, 85.6% of ambulance encounters resulted in an out-of-network bill, while 81.6% of ambulance encounters among patients who were admitted resulted in a surprise bill.
In both settings, emergency medicine and internal medicine were among the specialties that billed out-of-network most frequently.
Researchers noted that the study was limited by their inability to isolate which bills were unexpected, though they wrote that patients are likely to assume all physicians are in network at an in-network ED or hospital.
“Our findings are notable because out-of-network billing was common among medical transport services and hospital-based physicians … providing care at in-network hospitals,” researchers wrote. “In such circumstances, patients could easily assume that the entire hospital team is in-network and thus the balance billing may come as a surprise.”
They wrote that the findings may underestimate the extent of out-of-network billing because the study did not include billing from sources other than physicians and medical transport services, such as laboratory charges.